New tech 3-D prints ouchless COVID-19 vaccine patches
The tabletop printer could make this and other vaccines more accessible across the globe
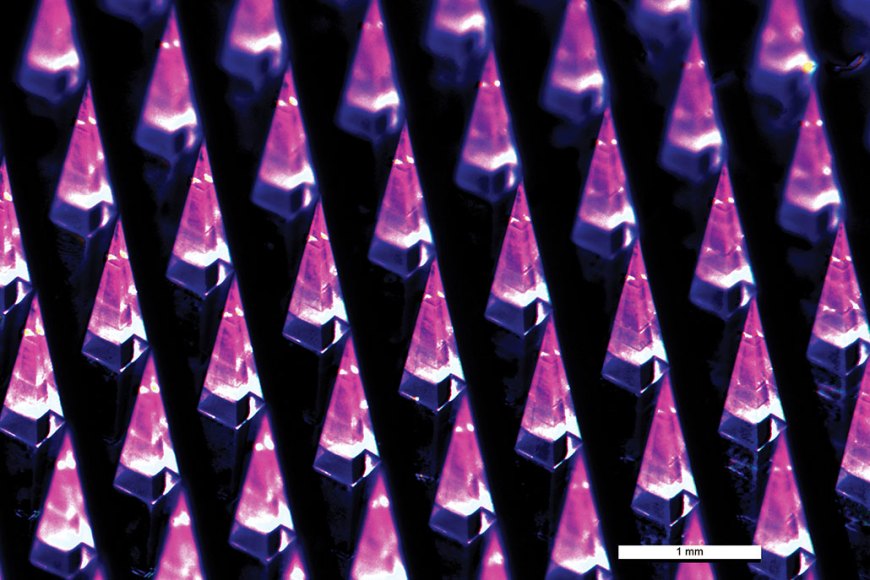
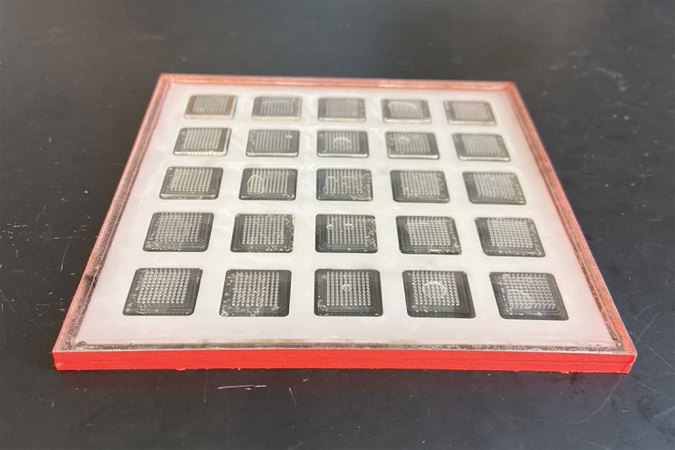
A new printer can produce COVID-19 vaccine patches, each with 100 microscopic needles (shown). The patches stick onto the skin. The needle tips dissolve within 10 minutes, after which the backing can be peeled off.
MIT (CC BY-ND)
Share this:
- Share via email (Opens in new window) Email
- Click to share on Facebook (Opens in new window) Facebook
- Click to share on X (Opens in new window) X
- Click to share on Pinterest (Opens in new window) Pinterest
- Click to share on Reddit (Opens in new window) Reddit
- Share to Google Classroom (Opens in new window) Google Classroom
- Click to print (Opens in new window) Print
Many people dread getting shots. The long needles used to reach muscle can leave many yelling, “Ouch!” But one day, the jabs used to deliver vaccines could be replaced by stick-on patches. Their tiny, dissolvable spikes are so short they’re basically painless. And a new tabletop microneedle-patch printer could help those ouchless vaccines reach more people.
Researchers described the innovative printer April 24 in Nature Biotechnology.
As part of this work, the scientists also developed a patch version of a COVID-19 vaccine. When tested in mice, it was just as effective as the traditional jab. And the patches can be stored for months at room temperature. The Pfizer and Moderna vaccines cannot. They must be stored at cold temperatures.
This new printer “potentially could revolutionize vaccination, particularly for children in the world’s poorest countries,” says Ryan Donnelly. He did not take part in the new study. But he does know about microneedle patches. He’s developing his own versions at Queen’s University Belfast in Northern Ireland.
How to print patches
Microneedle vaccine patches have been in the works for decades. One reason: “It’s a much gentler way to vaccinate than the syringe and needle,” says Ana Jaklenec. She’s an engineer at the Massachusetts Institute of Technology, in Cambridge. Sticking on a patch doesn’t really hurt. It feels like pressing the sharper, hook-filled side of Velcro onto your skin, she notes.
These patches can be manufactured using fancy machines. But Jaklenec wanted to lower their cost and make them more accessible, especially in low-income countries. So she and her colleagues developed a compact manufacturing machine.
The printer is about 120 centimeters long by 60 centimeters (four feet by two feet) wide and 60 centimeters tall. Inside it, a robotic arm dispenses special “inks” into molds similar to ice cube trays. To prevent air bubbles, a vacuum sucks the inks down into the microneedle-patch molds.
The first ink contains the vaccine. It fills the top half of the microneedle tips. It’s only these upper halves that “get through your skin and dissolve,” Jaklenec says. After that first ink layer dries, the printer dispenses a second, vaccine-free ink. It fills the base of the microneedles and forms the backing of the patches.
The prototype printer, which can make 100 patches at once, takes 48 hours per batch. Each patch contains 100 microneedles across a 1 square centimeter (about 0.4 square inch) base. These tiny needles are finer than a pencil tip, Jaklenec says. And they’re only 1.5 millimeters (0.06 inch) tall. That’s shorter than a strand of spaghetti is wide.
Engineers can build even larger versions of the printer, Jaklenec says. These could manufacture more patches at once or patches with more microneedles.
An ouchless COVID-19 vaccine
To test the printer, Jaklenec’s team developed its own version of a COVID-19 vaccine. It relies on messenger RNA — or mRNA — just like Moderna and Pfizer’s vaccines do. (The researchers created their own version because this project began before any COVID-19 vaccines were available. But the team’s formula turned out to be quite similar to one of Pfizer’s candidates.)
Several mice received two vaccine patches, applied four weeks apart. Three weeks after their second dose, these mice showed an immune response just as strong as mice that had received shots of the vaccine. However, mice that got the jab showed an immune response two weeks earlier than those that got the patches.
That delay might be because the patches start out as solids. Before the vaccine can enter the body’s cells, the needle tips must fully dissolve in the skin, Jaklenec explains. “So it takes a little longer for the mRNA to move about.”
The patches still showed they should work well in mice after being stored for six months around room temperature. In the study, that was 25° Celsius (77° Fahrenheit). When stored that way, the liquid vaccine didn’t remain as effective. (Pfizer and Moderna’s vaccines, for instance, require super-cold temperatures for long-term storage.)
Vaccines last longer in solid form, Jaklenec notes. Being solid prevents molecules from moving. That limits the chemical reactions that can break down the chemicals. So the solid patch is more stable. Liquid versions must be frozen to get the same effect.
The future of vaccines
People in low-income countries would likely benefit the most from this new vaccine printer, Donnelly says. To eliminate the risks associated with liquid vaccines, the vaccine patches could be produced as solids onsite. There would also be no needles to dispose of, he notes. And the patches could be administered by anyone, not just skilled healthcare workers.
But taking the vaccine production process out of a regulated lab setting brings new challenges, Donnelly says. Agencies like the U.S. Food and Drug Administration, he says, would need to validate the “safety, quality and efficacy of a vaccine … produced onsite in a remote environment.”
The new drug patches wouldn’t be limited to the COVID-19 vaccine. Scientists are investigating microneedle patches for flu and measles. They could even work for treating other species, including plants. When the printer project started, Jaklenec says, her group was going to work with a vaccine for Ebola. It’s a virus that has had outbreaks in Central and West Africa.
Vaccine patches — and this compact printer — seem promising. But it will take a long time for them to become widely used. First, they must win approval from health agencies.
Still, Jaklenec is hopeful these innovative patches will eventually make a difference. “There are many places where people don’t have really great access to health care,” she says. “So my goal is to develop things that can maybe help bring more equity in that space.”
This is one in a series presenting news on technology and innovation, made possible with generous support from the Lemelson Foundation.





