Gut bacteria may affect how well your medicines work
New research could help doctors choose drugs for patients based on their microbes
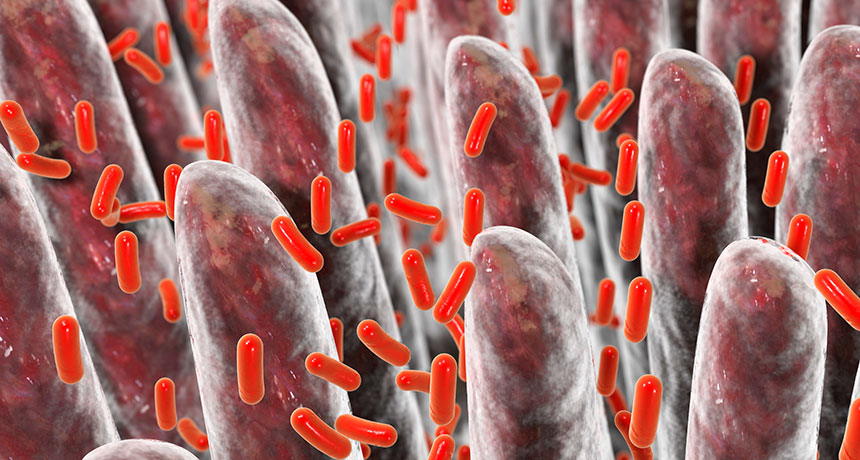
Bacteria living in your tummy (illustrated) could interfere with many oral medicines.
DR_MICROBE/iStock/Getty Images Plus
Share this:
- Share via email (Opens in new window) Email
- Click to share on Facebook (Opens in new window) Facebook
- Click to share on X (Opens in new window) X
- Click to share on Pinterest (Opens in new window) Pinterest
- Click to share on Reddit (Opens in new window) Reddit
- Share to Google Classroom (Opens in new window) Google Classroom
- Click to print (Opens in new window) Print
To prescribe the best medicine, it might help if a doctor knows which bacteria live in a patient’s gut. That’s the finding of a new study.
Reports had shown that some gut microbes can alter the drugs that people swallow. That might affect how well those drugs work. But researchers weren’t sure how big a problem this was. Now, a study suggests that gut bacteria can modify many drugs. And that means the genes in those microbes may predict how those drugs would work in that patient.
Maria Zimmermann-Kogadeeva is a computational biologist at Yale University in New Haven, Conn. She and her colleagues shared their new finding June 3 in Nature.
“Knowing how the gut microbes … affect a drug is hugely useful,” says Matthew Redinbo. He did not take part in the new research. But as a biochemist at the University of North Carolina at Chapel Hill, he understands that such effects could help drug companies develop more effective drugs. It could also help doctors choose the best treatment for a particular patient.
Researchers chose 76 types of bacteria that can live in the human gut. Then they tested if — and how — those bacteria changed the molecular structure of 271 drugs. From hormones to anti-virus drugs, each medicine had been designed to be taken by mouth.
The scientists put the bacteria into test tubes holding nutrients and drug solutions. After 12 hours, about two in every three of the drugs had been changed by at least one strain of bacteria. Each of these strains could modify between 11 and 95 different drugs.
“That is huge,” says Nichole Klatt. The microbiome is the sum of all of the microbes living in the body. Klatt is a microbiome researcher at the University of Miami in Florida. She, too, was not involved in the new study. Still, she notes, knowing which microbes affect which drugs isn’t enough. Future studies should look into exactly how bacteria make these changes, she says. Studies might also explore the impacts those altered drugs would have on the human body.
DNA detectives
Zimmermann-Kogadeeva and her colleagues wanted to know which part of a bacterium’s DNA lets it modify a particular drug. To find out, they first chopped up DNA from the germs of interest. Then they inserted individual snippets of that DNA into the cells of E. coli bacteria. Afterward, they watched to see which, if any, of these altered E. coli were now able to change the drugs. This told them which DNA fragments could mess with those drugs.
Next, the researchers did a series of tests using different drugs. They started by sampling feces from 28 people. Then they tested whether the community of microbes in each person’s poop could modify any of the drugs. In each test, they exposed all the microbial communities to the same drug.
The researchers also scouted in each stool sample for the drug-altering DNA snippets they’d found in the E. coli test. They searched, too, for bits of DNA from other microbes that were at least 50 percent similar to these germs genetically. Their idea was that similar DNA segments likely would do similar jobs.
Feces with more of the drug-altering DNA pieces made more changes to drugs, the team found. That suggests doctors could genetically test a patients’ poop before prescribing them medicine. Such stool tests might tell them whether a patient’s gut microbes would likely alter a drug they could be prescribed.
Such tests might one day help doctors choose which medicine to prescribe. Or doctors might prescribe a treatment that makes a person’s gut microbes friendlier to a certain drug. Antibiotics or fecal transplants might even become ways to change a patient’s gut microbes, says study coauthor Michael Zimmermann. He’s a pharmaceutical scientist and systems biologist at Yale.
But it’s important to consider, too, that the way germs mess with drugs “actually can be beneficial,” Zimmermann-Kogadeeva says. Drug companies might want to make drugs that take advantage of the ability of germs to make a drug work better, she says. Those companies might also design pills to avoid bad reactions with bacteria in the first place.







